Relationship between serum ghrelin levels, weight loss and quality of life in patients with advanced non-small cell lung cancer- Juniper Publishers
Juniper Publishers- Journal of Cell Science
Abstract
Cancer cachexia is one of the most frequent effects
of malignancy, is often associated with poor prognosis, and may account
for up to 20% of cancer deaths. The aim of our study was to evaluate the
relationship with serum levels of ghrelin, weight loss, and quality of
life in advanced non-small cell lung cancer patients.
Methods: A total of 67 chemotherapy-naïve
advanced stage non-small cell cancer patients enrolled to study.
Demographical, anthropometrical, laboratory data and serum levels of
ghrelin were measured. Progression-free survival and overall survival
were estimated using the Kaplan-Meier method. Survival among various
factors was calculated using the log-rank test. Patients quality of life
is evaluated with several questionnaires.
Results: Ghrelin levels were 4.6 - fold
(p=0.009) higher among patients with weight loss at the time of
diagnosis. Lower serum levels of ghrelin were associated with better
progression-free survival (p=0.011).
Conclusion: Serum ghrelin levels play key role
as proinflammatory cytokines in lung cancer and weight loss; however,
their use as diagnostic or prognostic markers is not possible yet and
further large-scale studies are required to confirm our findings.
Keywords: Non-small cell lung cancer; Ghrelin; Weight loss; Quality of lifeIntroduction
Cancer cachexia is a complicated catabolic process
which affects approximately two thirds of cancer patients and is caused
by a systemic cascade in which many cytokines and mediators play role
[1]. These mediators are often released by tumor cells. Cachexia
development in cancer patients decreases treatment response and worsens
tolerance, and thus affecting survival and quality of life [2]. Cancer
cachexia may account for up to 20% of cancer deaths [2]. In a study
conducted on prognostic value of weight loss, it was determined that
weight loss was present in 59% of cases with small cell lung cancer, 58%
of cases with non-small cell lung cancer (NSCLC), and 76% of cases with
mesothelioma before the initiation of treatment [3].
Ghrelin is also named as appetite hormone [4].
Seventy percent of ghrelin is produced by X/A cells which are present in
oxyntic mucosaand have endocrine logical functions. Ghrelin is a strong
orexigenic (increasing appetite) molecule [5]. Ghrelin increases protein
synthesis and carbon hydrate utilization, but it decreases fat
utilization, so that energy gain and storage are performed [5]. Plasma
ghrelin level is indirectly proportional to body mass index (BMI).
Ghrelin level is increased in negative energy equilibrium [5]. The role
of ghrelin in cancer and cancer induced cachexia is unknown. It is
believed that ghrelin levels in cancer patients may be increased due to a
systemic inflammation, and as a compensatory mechanism to catabolic
process.In the present study, we aimed to reveal serum ghrelin levels in
patients with advanced NSCLC, and its role in weight loss, and to
evaluate its effects on quality of life as well as whether this peptide
is a prognostic biomarker for cachexia.
Materials and Methods
Subjects
A total of 67 chemotherapy-naïve patients who were admitted
to Medical Oncology Department for the first time and were
pathologically diagnosed as NSCLC were evaluated. A written
informed consent was obtained from each participant. The
study protocol was approved by the Medical Ethics Committee
of Pamukkale University Medical Faculty (No: 02 / Date:
24.02.2009). The study was conducted in accordance with the
principles of the Declaration of Helsinki.The patients at advanced
stage (Stage IIIB and Stage IV) whose performance status (PS)
was 0, 1, 2 according to the World Health Organization (WHO)
classification were included in the study. The patients whose PS
was 3 and worse on admission, those with cranial metastasis
or suspicion of cranial metastasis, patients aged 80 and above,
those at early stage (I, IIand IIIA), those the patients who were
unwilling to give a written informed consent and who refused
to answer the questionnaire were excluded from the study.Age,
sex, anthropometric measurements, type of tumor, treatment,
and the pre-treatment performances of the patients were
recorded. The presence of weight loss at the time of diagnosis
was questioned. Weight loss at the time of diagnosis was defined
as a loss of more than 10% within the past six months.
Biochemical analysis
Blood samples were taken before treatment in the patient
group and blood samples were taken between 08:00 and
09:00 A.M. following an 8-12 hour fasting. A complete blood
count was measured using the CELL-DYN 3700 Systems and
CELL-DYN Sapphire device. Ferritin, C – reactive peptid (CRP),
glucose, insulin, and cortisole, albumin was measured with
Roche/Hitachi Cobas c Systems, e 601 Module device. For
the analysis of insulin resistance, the Homeostasis Model
Assessment (HOMA-IR, Homeostasis Model Assessment) tool
which provides practical examination of beta-cell function
and insulin resistance using fasting glucose and insulin levels
was used. It was calculated as fasting insulin value (μIU/mL) x
fasting glucose level (mg/dl)/405. In healthy individuals, HOMA
value is lower than 2.7, while values above 2.7 indicates insulin
resistance [6].Furthermore, 6ml of venous blood samples were
taken from patients, for ghrelin analysis and the samples were
taken to vacuumed tubes and the samples were centrifuged
at 15,000rpm for 10 minutes. Serum was, then, separated and
stored in a deep freezer at -70°C. It was measured by Enzymelinked
immunosorbent Assay (ELISA) method (Digital and
Analog System, DAS, Plombara Sabina, Italy). The cut-off value
of ghrelin was calculated using an automatic program. The cutoff
value for ghrelin was 1275pg/ml. The values at and below
this value were evaluated as low and the values above this value
were evaluated as high.
Questionnaires
Patients’ quality of life was assessed by conducting a
questionnaire and nutritional status were assessed by subjective
global evaluation concurrently with blood sample collection.
European Organization for Research and Treatment of Cancer
Quality of Life Questionnaire (EORTC-QLQ-C30) the validity
and reliability of the Turkish version of European Organization
for Research and Treatment of Cancer Quality of Life (EORTCQLQ-
C30) (version 3) was performed previously [7]. This tool
is widely used in cancer patients all over the world. The scale
evaluates health status and quality of life. On the function scale,
there are questions about physical function, role function,
emotional function, comprehension function, and social
function; and functions to sustain daily activities are inquired. On
the symptom scale, fatigue, nausea and vomiting, pain, dyspnea,
insomnia, loss of appetite, constipation, diarrhea, and financial
status are inquired. The last two questions represent the general
health status scaleand show patients’ self-assessment on quality
of life as a whole. Functional, symptom, and general health status
scores of the patients in EORTC-QLQ-C30 were determined
with a scoring guideline created by using formulas [8]. Higher
functional and general health status scores and lower symptom
scores indicates a better quality of life for the patients.
Quality of life questionnaire, short form 36 (SF-36)
Short form 36, has a generic measurement characteristic
among quality of life questionnaires and provides a wide range
of measurement; it has been developed by Rand Cooperation
and the validity and reliability studies of the Turkish version
has been performed previously [9]. It is a self-assessment scale.
Lower score indicates poor health status, whereas higher score
indicates good health status.
Hospital anxiety and depression (HAD) scale
Hospital anxiety and depression scale has been specifically
developed to use in hospital settings. It is a self-assessment scale
to determine the risk of anxiety and depression and measure the
level and change in the severity of them in the patient. The scale
has been applied to various diseases, and compared between
clinical groups, and it is shown that it indicates clinically
significant results as a screening tool [10]. HAD scale has been
translated into Turkish and the validity and reliability studies
of the Turkish version has been performed, and it has been
reported as a suitable tool in Turkey [11].
Statistical Analysis
Statistical analysis was performed by SPSS-16.0 for windows
package program. Results were evaluated at a confidence
interval of 95%. The level of statistically significance was
accepted as p<0.05. Spearman and Pearson correlation test was
used in correlation analyses. Kaplan-Meier method was used for
overall survival (OS) and progression-free survival (PFS) curves.
Logistic regression was used for analysis of factors affecting
survival and progression.
Result
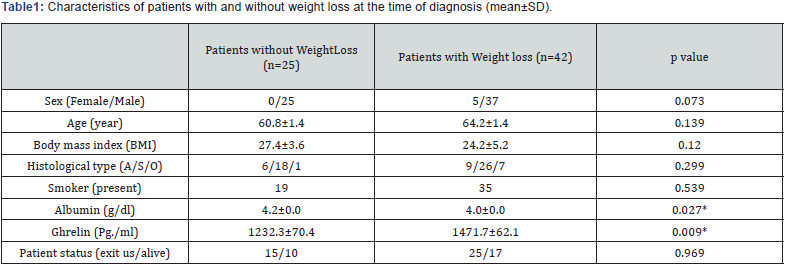
A total of 67 patients diagnosed with advanced (stage
IIIb and IV) NSCLC were included in the study. Of patients, 62 92.5%) were males, and 5 (7.5%) were females. Patients were
divided into two groups according to weight loss at the time of
diagnosis. The main clinical and demographic characteristics of
patients with and without weight loss at the time of diagnosis
are shown in (Table 1).Ghrelin levels were 4.6-fold (p=0.009)
higher among patients with weight loss at the time of diagnosis,
calculated with Mann Whitney U test. No significant difference
was found between ghrelin and sex, PS, smoking, anemia, CRP,
ferritin, cortisole, albumin levels, and IR.
Patients with low ghrelin levels, physical (p=0.004) and role
(p=0.015) function scores of EORTC-QLQ-C30 subscales and
physical function (p=0.006), pain (p=0.004), and mental function
(p=0.003) scores of SF-36 subscales were measured higher;
fatigue (p=0.002) and pain (p=0.023) scores of EORTC-QLQ-C30
subscales were found higher. Besides, in these patient’s anxiety
(p=0.023) and depression (p=0.016) scores in HAD scale, and
nutritional status (p=0.026) scores were normal.
When subscales of EORTC-QLQ-C30 and SF-36 questionnaires
were examined, physical (p=0.008, and p=0.032, respectively)
and role function (p=0.009, and p=0.048, respectively) scores
of patients with weight loss at the time of diagnosis were lower
than those without weight loss. Fatigue (p=0.010), dyspnea
(p=0.032), and loss of appetite (p=0.013) scores of patients who
had weight loss at the time of diagnosis were higher. However, no
correlation was determined between HAD, nutritional condition
questionnaires, and weight loss. On a subscale of EORTCQLQ-
C30 questionnaire, physical function scores were lower in
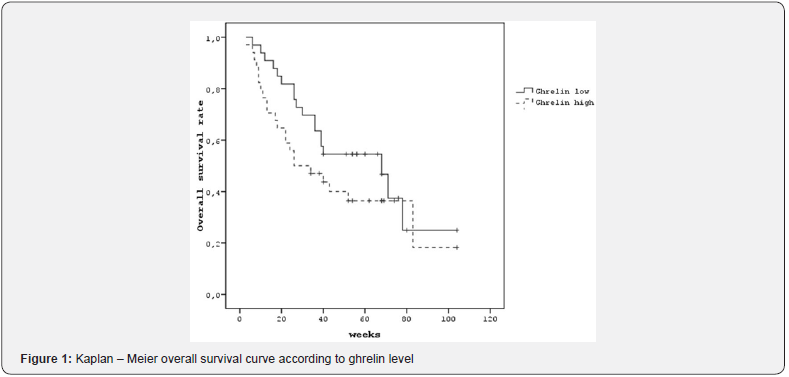
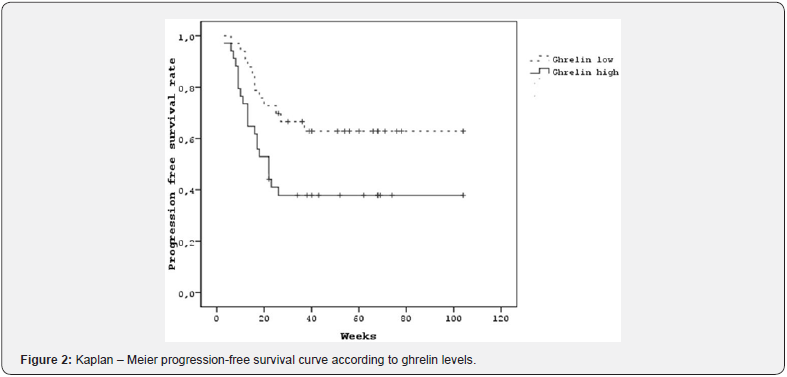
patients with lower albumin levels (p=0.006).Patients with low ghrelin levels had the median of OS was 68 weeks, and it was 26 weeks in the patients with high ghrelin levels; however, the difference was not statistically significant (Figure 1). Among patients with high ghrelin levels, the median PFS was 22 weeks, whereas it could not be reached in patients with low ghrelin levels (p=0.023) (Figure 2).
Discussion
Ghrelin is an orexigenic hormone, and it antagonizes leptin
which decreases food intake [12]. Serum leptin levels were found
significantly lower in lung cancer patients than healthy controls
[13]. It is believed that ghrelin administration antagonizes effect
of cytokines which act on appetite and weight loss [14]. Ghrelin
levels are positively correlated with cachexia conditions like
anorexia nervosa [15], chronic obstructive pulmonary disease
[16] and end stage renal disease [17]. Ghrelin levels have been
found lower in weight gain and obesity [15]. It was suggested
that role of ghrelin in inflammatory process of cancer was
cytokine inhibition, and it had also ant proliferative effects[18].
It was thought that ghrelin levels were increased through
compensation caused by its anti-inflammatory effects.
In our study, ghrelin levels were found higher in patients who
had weight loss at the time of diagnosis. It might be considered
that increased ghrelin levels in cachectic patients were due to
compensation of the catabolic process [19]. This hypothesis was
supported by another study performed on patients with lung
cancer (20). Basal ghrelin levels were determined significantly
higher in cache tic patients, and it was observed that ghrelin
levels were significantly increased in patients whose food
intake was decreased on days 8 and 21 after chemotherapy
[20]. These results indicated that anorexia might affect ghrelin
levels in patients with lung cancer. In the same study, there was
a correlation between PS and ghrelin, and ghrelin levels were
measured significantly high in patients with poor PS [20]. In our
study, only basal ghrelin levels were measured, but ghrelin levels
after chemotherapy were not measured. Also, no correlation was
found between PS and ghrelin levels.
It was thought that ghrelin might be increased to compensate
anorexia, and short-term appetite loss, fasting, and re-starting
food intake might affect ghrelin levels. Although ghrelin level is
high in anorexic patients, and high ghrelin levels are expected
to increase appetite, it is observed that these patients have
loss of appetite. The possible cause of this loss of appetite is
that, similar to insulin resistance mechanism, although ghrelin
concentration is high in the blood, there may be a loss of ghrelin
receptor affinity. Karapanagiotou [21] found that ghrelin levels
were higher in the advanced NSCLC patient group. Studies
performed on patients with lung cancer, ghrelin levels were
higher in-patient groups than control subjects, however there
was no statistical significance [20,21]. Basal ghrelin levels of
patients with and without weight loss before chemotherapy
were measured in 101 patients with advanced lung cancer and
60 healthy controls by Karapanagiotou [21].
Weight loss was observed in 75 patients, whereas
there was
no weight loss in 26 patients. Ghrelin levels were determined
significantly higher in patients with weight loss at the time of
diagnosis. In the same study, no correlation was determined
between ghrelin levels and age, cancer stage, histological type,
PS, PFS, and OS rates. It was underlined that OS rates were lower
in patients with low BMI and poor performance despite an
insignificant difference. In our study, ghrelin levels increased 2.8-
fold in patients with progression. No correlation was determined
with OS.In a study performed on 14 breast cancer cases and 26
colon cancer cases, and 20 healthy controls, patients were divided
into two groups as cache tic and non-cache tic. Ghrelin levels
were found significantly higher in cache tic patients. Ghrelin
levels in cache tic female patients were significantly higher
than the levels in male patients [22]. In our study, there was no
correlation between sex and ghrelin levels, but low number of
female patients (n= 5) might be an effective factor in this issue.
Jeon [23] compared sixteen cache tic patients with advanced
gastrointestinal cancer (2 with esophagus, 9 with gastric, and 5 with
colorectal cancer), and ten healthy controls.Ghrelin levels
were found significantly higher in cachectic patients, whereas
no correlation was determined with BMI. The main tissue for
ghrelin secretion is stomach, and it has been shown that ghrelin
levels decreased after gastrectomy. In that study, 7 patients
had total gastrectomy, but no significant difference was found
in ghrelin levels in patients with and without gastrectomy [23].
This condition was explained as ghrelin secretion from other
tissues (T cells, spleen, thymus, and intestines) could increase
after gastrectomy by the compensatory secretion.
In a study performed in cache tic gastric, pancreatic
and colorectal cancer patients, ghrelin levels decreased
significantly[24]. This suggests our minds that there might be
other special effects on ghrelin production in patients with
gastrointestinal cancers. Therefore, it was reported that patients
with gastrointestinal cancers might be the most suitable group
for exogenous ghrelin administration. In a phase II, placebocontrolled,
randomized study, ghrelin was administered to cache
tic and non-cache tic tumor implanted rats, and 30% elevation
was reported in appetite and food intake [25]. Again, in a doubleblind,
randomized, placebo-controlled study carried out on
cache tic rats with cancer, favorable results of exogenous ghrelin
administration were reported [26].
The present study and the other studies suggest that ghrelin
has a compensatory role in pathogenesis of cancer cachexia,
and it shows its effects through mediators affecting a systemic
inflammation rather than mediators affecting fat metabolism.
The small sample size and lack of ghrelin measurements
after chemotherapy are limitations of this study. This study
demonstrated that ghrelin levels were found to be higher in
patients with weight loss at the time of diagnosis. Serum ghrelin
levels are important in cancer and cancer cachexia; however,
the utilization of ghrelin as a diagnostic or prognostic tool is
not possible yet and further largescale studies are required to
confirm our findings.




Comments
Post a Comment