The Oleaginous Rucksack-Steacystoma Multiplex-Juniper Publishers
Juniper Publishers- Journal of Cell Science
Preface
Steatocystoma multiplex was preliminarily cogitated by Jamieson in 1873 and cogent nomenclature was instituted by Pringle in 1899. Terminology is composed of the literal meaning of steato and cyst as a “bag of fat” whereas multi and plex are delineated as “network”. An exceptional, hamartomatous cutaneous disorder engendered by the pilosebceous unit with characteristic multiple, asymptomatic, skin coloured nodules and constituted of dermal cysts impacted with sebum is denominated as steatocystoma multiplex. Facial variant of steatocystoma multiplex is enunciated which concurs with disorders such as eruptive vellus hair cysts, trichofolliculoma and epidermoid cysts [1,2].
Disease Characteristics
Incriminated sites commonly incorporate zones of mature, well developed pilosebaceous units or an augmented quantification of sebaceous glands such as trunk, neck, axilla, groin scalp, proximal extremities, face, buttocks, breast and forearm, although no location is exempt. An autosomal dominant mode of disease inheritance is cogitated although sporadic instances can be discerned. The disorder has an equivalent gender distribution. The condition is frequent in adolescence or early adulthood with a mean age of emergence at 26 years. Hormonal variations can activate the lesions which develop and enhance briskly in neonates, middle aged and elderly individuals. Additionally, trauma, infection and inadequate immune response are implicated in genesis of the cysts. Steatocystoma multiplex suppurativa as a subcategory can depict inflamed cysts which rupture subsequently to produce secondary infection and configuration of abscesses. Steatocystoma multiplex can be considered synonymous with polycystic disease of the epidermis and sebocystomatosis [2,3]. Isolated, singular lesions of steatocystoma are enunciated as steatocystoma simplex. Keratin 17 is a cogent intermediate filament located in the epithelial cells of nail bed, hair follicles and sebaceous glands. An acral arrangement of lesions indicates a deranged keratin 17 gene, usually accompanied by ectopic sebaceous glands. Pachyonychia congenita, particularly the variant pachyonychia congenita KRT17 or the erstwhile pachyonychia congenita type 2 and steatocystoma multiplex are associated with genetic mutation of keratin 17. Steatocystoma multiplex is contingent to eruptive vellus hair cysts, a condition which is contemplated as a continuum to the pathologic disease process [2,3].
Clinical Elucidation
Cysts are cogitated in multitudinous regions such as the chest, head and neck, face, scalp, abdomen, gluteal region, breast, skin flexures and arms. Innumerable, firm to elastic, mobile, recurrent, asymptomatic, painless, non-pruritic, cystic or dome shaped, gradually progressive, skin coloured nodules or papules of soft consistency and magnitude varying from 0.5 centimetres to 3.0 centimetres are elucidated at various sites. Rarely, nodules or plaques can appear to be dark blue or calcified. The extraneous surface is smooth, and cysts contain oily, yellowish to cheesy, semisolid substance which can be extracted through the centric punctum. Steatocystoma multiplex can be classified into generalized, localized, acral, facial, flexural, suppurative and syndromal variants. Additionally, steatocystoma multiplex infrequently incorporates variants such as papular, steatocystoma multiplex conglobata, accompanied by foreign body granuloma or as linearly configured lesions [3,4].
Genetic Transformation
Genomic mutation of R94C delineating guanine to adenosine (G to A) genetic transition is discerned within base 428 of 94th codon, which constitutes the keratin 17 gene, in subjects of steatocystoma multiplex. The mutated allele is devoid of enzyme cutting locus thereby producing an uncut chromosomal band with 200 base pairs (normal subjects depict dual chromosomes of 108 base pairs and 92 base pairs each). A heterogeneous mutation c.280C/T(R94C) situated in exon 1 of keratin 17 gene is delineated in familial settings of steatocystoma multiplex. Additionally, mis-sense mutations at locales R94H and N92S are discerned in steatocystoma multiplex arising in Asian subjects. Aforesaid mutations disrupt the configuration of keratin intermediate filaments [4,5].
Associated Conditions
Cysts of steatocystoma multiplex can coexist with epidermal vellus hair cysts, trichofolliculoma, trichostasis spinulosa, pilomatrixoma and epidermoid cysts. Amalgamation of aforesaid cysts can occur concomitantly, asynchronously or hybrid cysts can emerge. Attributes cogitated by cysts of steatocystoma multiplex and eruptive vellus hair cysts are identical such as mode of disease inheritance, age of onset, pattern of distribution, morphological features and localization of cysts within the mid dermis on histology. Steatocystoma multiplex is concurrent with eruptive vellus hair cyst, persistent infantile milia and epidermoid cysts as a continuum of the disease spectrum. Histological elucidation is characteristic and diverse. Cyst wall is constituted of sebaceous lobules or mature sebaceous glands in steatocystoma multiplex and vellus hair follicles in eruptive vellus hair cyst. Cyst content is divergent, composed of oily and cheesy substance in steatocystoma multiplex and vellus hairs elucidating mesh incorporated strands and hair in eruptive vellus hair cysts. Thus, histogenesis of concordant entities such as eruptive vellus hair cyst and steatocystoma multiplex is common and emerges from the pilosebaceous unit with diverging differentiation. Syndromal steatocystoma multiplex exemplifies specific, associated syndromes [5,6]. Immune expression of K17 is delineated in pachyonychyia congenita, a condition which manifests as oral leukokeratosis, palmo plantar keratoderma, follicular hyperkeratosis, generalized steatocystoma multiplex and eruptive vellus hair cysts. Association is contingent with the X linked recessive Lowe’s syndrome or the oculocerebrorenal syndrome constituted by cataracts, hypotonia and renal dysfunction. Gardner’s syndrome, also termed as familial adenomatous polyposis syndrome, demonstrates innumerable cysts such as epidermal, dermoid, infundibular and steatocystomas. Steatocystoma multiplex is a component of Noonan’s syndrome or LEOPARD syndrome along with lentiginosis, ocular hypertelorism, stunted growth, genital anomalies and deafness. Steatocystoma multiplex appears in concurrence with Alagille Watson syndrome which implicates the heart, musculoskeletal and hepatorenal system. Favre Racouchot syndrome which demonstrates solar elastosis, comedones and infundibulofollicular cysts, are concomitant with syndromal steatocystoma multiplex [6,7].
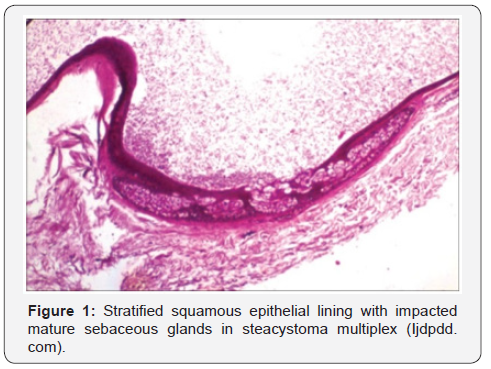
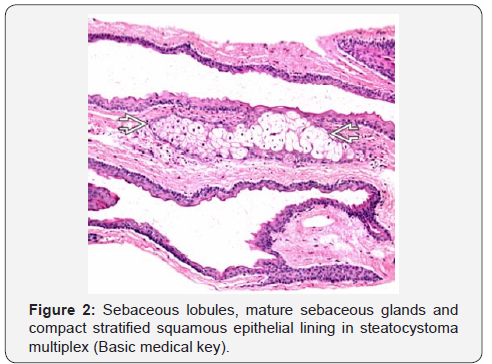
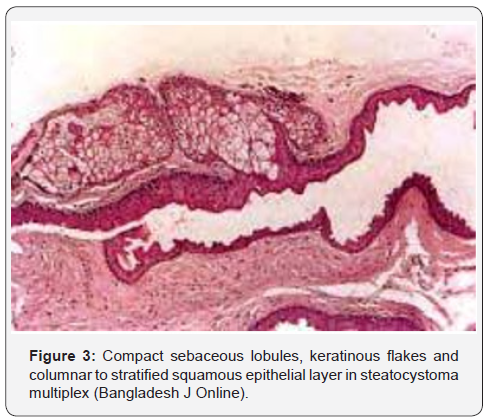
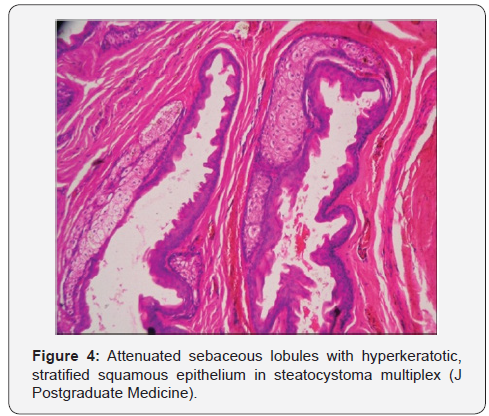
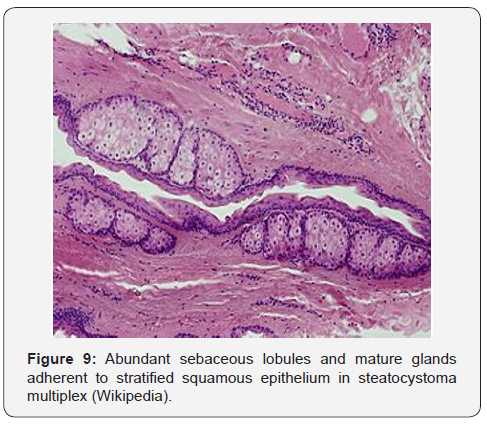
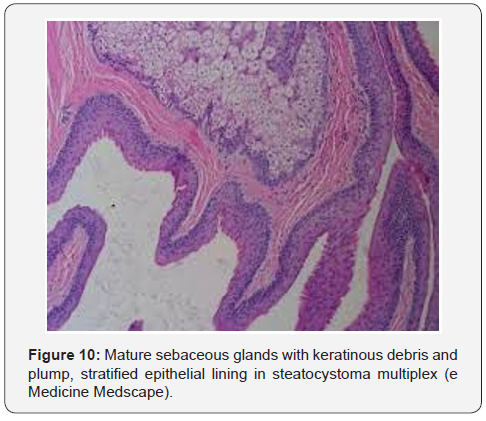
Histological Elucidation
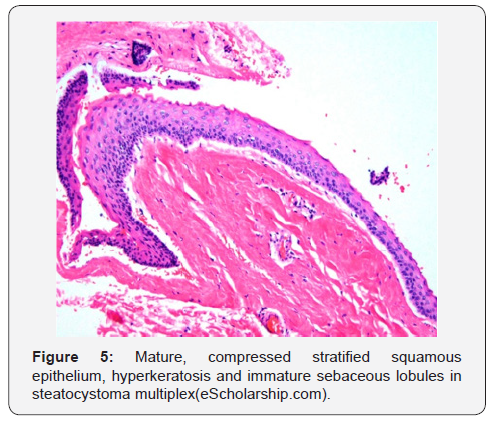
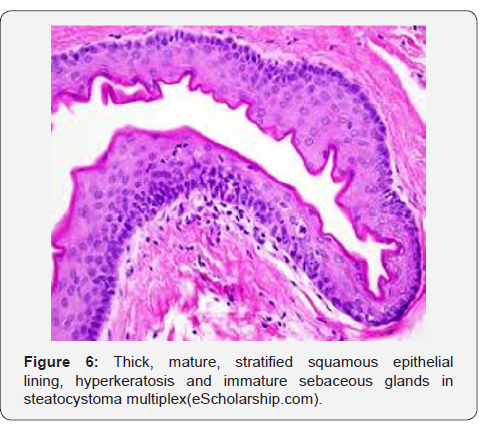
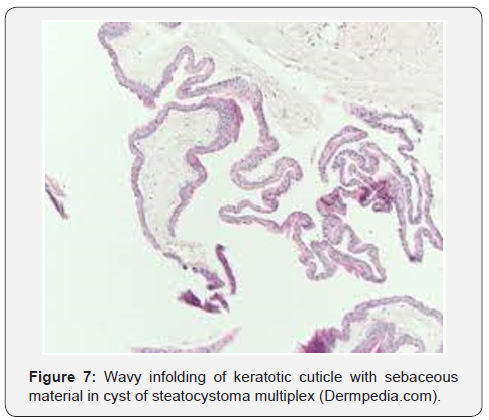
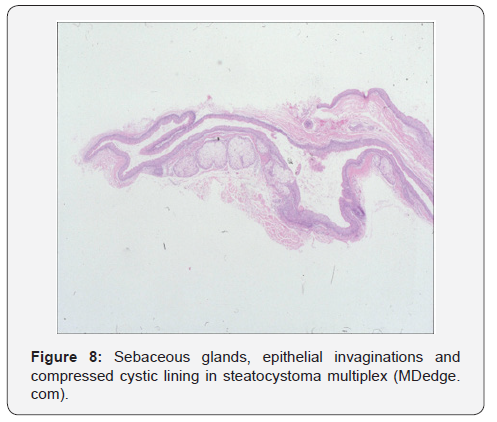
Steatocystoma multiplex is classically a tumour of the naevoid duct and sebaceous glands. The neoplasm is engendered from sebaceous follicles. A continuum with superimposed epidermis is achieved with an epithelial cord which is essentially a remnant of follicular infundibulum. The infundibulum frequently encloses sebocytes. Infundibular cord with cogent lumen is impacted with cellular debris derived from keratinocytes, corneocytes, sebocytes or accumulated hair. Cysts of steatocystoma multiplex are predominantly situated within the mid-dermis. Cysts are typically lined by two to three layers of stratified squamous epithelium and are characteristically devoid of a granular cell layer. Additionally, a dense, homogenous, eosinophilic, undulating cuticle with an intricate, folding configuration displays sharp invaginations into the cystic cavity, which is impacted with an amorphous, eosinophilic, keratinous debris. Stratified squamous epithelium layers the cyst wall which contains or displays abutting sebaceous lobules or flattened sebaceous glands. Multinucleated giant cells and chronic lymphocytic infiltrate are cogitated within the cyst wall along with enlarged cells with granular cytoplasm appearing adjacent to typical epithelial lining cells of steatocystoma multiplex [7,8]. Superficial epidermis is typically normal and demonstrates middermal or exceptionally, subcutaneous cysts. Infrequently, a sebaceous adenoma can assimilate within the cyst wall, thereby exemplifying a terminology of “steatosebocystadenoma”. Cyst wall can collapse on account of histological processing with consequent elimination of sebum and lipids. As a few cysts lack the typical histology of steatocystoma multiplex or do not adequately enunciate cogent pathogenic alterations, analysis of a singular tissue specimen can be inadequate and examination of multiple histological specimens or sections is recommended [2,4] (Figure 1-10).
Immune Histochemical Assay
Cysts are traditionally layered with mature, stratified squamous epithelium and display diversely configured subtypes of keratin. Squamous epithelium cogitated within steatocystoma multiplex elucidates various keratins such as keratin10 and keratin17. In contrast, eruptive vellus hair cysts singularly demonstrate immune reactive keratin17 and epidermoid cysts enunciate immune reactive keratin10 [2,3].
Differential Diagnosis
Distinction of steatocystoma multiplex is necessitated from conditions such as multiple epidermal cysts, lipomatosis, milia, sebaceous hyperplasia and sebaceous adenoma. Eruptive vellus hair cysts, xanthomatosis, neurofibromatosis and syringoma are associated conditions requiring segregation. Steatocystoma multiplex conglobata necessitates a demarcation from hidradenitis suppurativa, acne conglobata and retinoid resistant acne vulgaris. Pulmonary adenocarcinoma metastatic to the skin can be misdiagnosed as steatocystoma multiplex [9,10]. Mammary incrimination of steatocystoma multiplex can be misinterpreted as adjunctive lesions of the breast. Mammographic elucidation of steatocystoma multiplex demonstrates well circumscribed, spherical, radiolucent nodules with an attenuated, radio dense perimeter. Ultrasound exhibits an intra-dermal hypo-echoic or iso-echoic nodule or lesions with admixed echoes, debris and fluid levels. A cogent family history, imaging features and prominent, bilateral, spatial configuration of steatocystoma multiplex nodules is confirmatory. The terminology of sebaceous cyst ideally represents a true cyst, as is cogitated by steatocystoma multiplex [9,10].
Investigative Assay
Fine needle aspiration cytology is conducted to diagnose the condition. Material aspirated by a fine needle is composed of a yellowish, dirty fluid with crystalline configuration, amorphous debris, anucleate squames and squamous epithelial cells. The procedure is painless, can be performed in the physicans’s office and is devoid of scarring. Polarized and non polarized dermatoscopy can be performed to adequately diagnose the condition. Polarized dermatoscopy exhibits lesions with a distinctive, yellowish glow and an enveloping, darkly dispensed periphery which is super-imposed upon a pseudo-reticular pigmentary configuration. Vellum hair entrapped within the cystic cavity induces a greenish discolouration to the yellowish zones. Non polarized dermatoscopy demonstrates a yellowish, amorphous, structure-less zone with an inconspicuous perimeter, contingent to the sebaceous content of cystic lumen. Electron microscopy can suitably discern the histogenetic induction of steatocystoma multiplex. Cyst wall differentiates along the sebaceous ducts. An attenuated, keratinous lining of the cyst lumen, composed of elongated and flattened cells is cogitated. A circumscription of stratified squamous epithelium with basally situated columnar cells in preliminary lesions is exemplified. Basal cells gradually become shorter in chronic lesions [8,10]. Wavy, infolded, cuticular horn layer and immature sebocytes confined to the cyst wall are demonstrated. Aforesaid morphological attributes can segregate the cysts of steatocystoma multiplex from alternative conditions. Antecedent lesions depict keratohyaline granules and chronic lesions demonstrate retrogression with a consequent, characteristic absence of granular cell layer. Foci of sebaceous differentiation frequently concurs with variations of trichilemmal, pilomatricomal and infundibular subcategory of keratinisation.
Therapeutic Options
Untreated cysts of steatocystoma multiplex can exhibit complications, particularly hypertrophic and atrophic kind of scarring, thus recapitulating scarring elucidated in nodulocystic acne and hidradenitis suppurativa. Diverse therapeutic options are applicable for managing the disorder. Therapy is primarily a surgical intervention and comprises of modalities of aspiration of cyst content, cold steel surgery, cryotherapy, radiofrequency ablation and ablative lasers. Instances with therapeutic intervention of an intact cyst exhibit an augmented relapse of steatocystoma multiplex. Surgical extermination can be challenging in subjects with extensive, innumerable cysts. Cyst is incised with a vein hook and a sequential application of mosquito forceps to extract the cyst contents. Post inflammatory hyper-pigmentation can appear temporarily although reoccurrence is absent. Innumerable cysts of steatocytoma multiplex can be managed with oral antibiotics, incision and drainage and electrocautery under general anaesthesia. Cysts can be eliminated with simple incision and drainage or incision and drainage with sequential electrodessication for superior cosmetic outcomes [3,4]. Lesions administered local application of tricholoracetic acid following incision and drainage are accompanied by excessive irritation. Cryotherapy is adopted for managing enlarged or calcified lesions. However, the therapy is associated with procedural pain, blisters, hypopigmentation, scarring, hyper-pigmentation, inferior cosmetic results and reappearance of lesions. Cryotherapy can be employed for managing non-inflamed lesions of steatocystoma multiplex suppurativa. Ablative modalities such as carbon dioxide laser can be adopted for treating multiple lesions. Carbon dioxide laser is a technique which is minimally invasive, demonstrates satisfactory cosmetic results with a minimal reoccurrence rate. Laser vaporizes the cyst wall and ensuing remnants. Carbon dioxide laser can be employed to perforate cyst wall, contents are scooped, and the cyst heals by secondary intention. Lasers are an expensive therapeutic modality. Complications incorporate minimal scarring and hypo-pigmentation [10,11].
Radio-frequency ablation in combination with surgical eradication of the cyst wall is a preferred therapeutic modality. Radiofrequency is employed under local anaesthesia for miniature incisions within the cysts. Cyst contents are eliminated manually and subsequently the cyst sac is extracted. Healing occurs with secondary intention and aesthetic outcome is superior, devoid of scarring or post inflammatory hyperpigmentation. Cyst reoccurrence is negligible with aforesaid methodology. Administration of oral retinoids can be adopted, however the methodology demonstrates an elevated cyst reoccurrence with minimal benefits. Inflamed and suppurative lesions are appropriately managed with isotretinoin exhibiting specific anti inflammatory effects. Inflamed, cystic lesions are suitably treated with isotretinoin, although exacerbations occur. Non inflamed cystic lesions are unaltered with isotretinoin. Close monitoring is necessitated to evaluate the incidence of cyst reappearance. There remains a lack of consensus on optimal therapeutic strategies. Extent of disease with personal preference are crucial in pursuing cogent therapeutic strategies. Thus, a personalized therapeutic protocol is preferred for treating steatocystoma multiplex [11].




Comments
Post a Comment